Sim Center
A robotic simulator, or a manikin that sweats, sheds tears, has a heartbeat, and pulse. An imaging table that allows you to view skin, muscles, organs, and veins at any angle and to any depth. Detailed, unscripted interactions with “patients” in a serious form of improv theater.
That’s just some of what you’ll find at St. Luke’s Simulation Center. It’s a place where doctors, nurses, and others can sharpen existing skills (or learn new ones), as well as practice their patient-doctor interactions in a safe environment.
“Simulation is an essential part of medical training,” says Megan A. Augustine, M.Ed., Director of Network Simulation. “Until 2014, we had separate spaces dedicated to the school of medicine and the school of nursing.” Word began to spread of the benefits simulation had on education throughout the network, and attendance at the Sim Center grew from 3,700 people in 2014 to over 12,000 in 2018.
Many of us are familiar with golf simulators—devices that help you improve your game without setting foot on an actual course.
And so it is with the Sim Center. Lifelike models help learners acquire proper techniques for inserting a chest tube, delivering a baby, making an incision, and other procedures without the risk of harming an actual person. “If you make a mistake,” Augustine said, “you’re in a safe, controlled environment, and will get immediate feedback from your instructor.”
Properly called human patient simulators (HPS), they can imitate breathing, sweating or tearing, exhibit a pulse, and demonstrate a range of symptoms. They’re connected to medical monitors that present EKG, blood pressure, oxygen uptake, even lab results, and radiology reports.
Their programmed responses to “treatment” can also push learners to react professionally and quickly to unexpected situations.
“Learners can deliver a simulated premie or newborn baby from a birthing simulator. We can also program the birthing simulator to have a medical emergency—hemorrhaging for example—so the learner suddenly has two patients that need immediate attention,” Augustine explained.
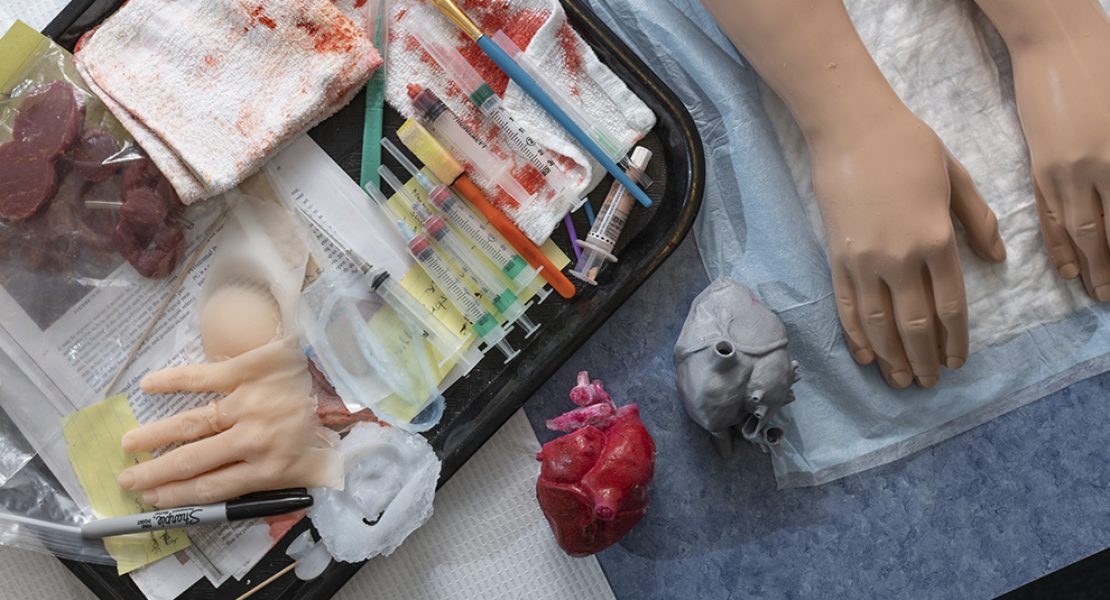
The center also features a GI Bronch Simulator and a Mimic dV-Trainer®, sophisticated simulators that replicate the action and “feel” for users to improve their bronchoscopy, GI skills, and robotic surgical skills. On a smaller scale, learners also use body part simulators (“task trainers”) to practice inserting arterial lines, performing intramuscular injections, inserting catheters, treating foot ulcers, and many other procedures.
In 2017, St. Luke’s realized that its large class sizes combined with its limited number of task trainers meant that more resources were needed. The cost-saving solution? Making those items in house.

Thanks to the St. Luke’s Auxiliary, the Sim Center purchased a 3D printer and other materials, enabling the facility to produce its own devices for injections; inserting peripherally inserted central catheter (PICC) lines; treating foot and leg ulcers, abscesses, pressure wounds, hand trauma; suturing, caring for ostomy stomas, and lots more.
“Since 2017, when the Sim Center began to make our own task-trainers in house, we have saved over $40,000,” Augustine said. “Those items are costly to buy, and we use a lot of them. “But making the trainers in house also gave us an additional benefit; we can produce trainers to our own specifications, instead of relying only on what’s commercially available, and do it quickly.
For example, the wound department asked for specific simulated deep wounds and pressure wounds, and a stomach for ostomy training. We produced exactly what was needed.”
In May, the Center purchased an Anatomage table, which enables learners to see highresolution 3D images of external and internal anatomy. “Data from four fully scanned human cadavers are in its memory,” Augustine said.
“Learners can call up the images, isolate portions of them if desired, rotate them in any direction, remove the skin, extract an organ—it’s essentially a virtual dissection table.”
But medical training involves more than acquiring clinical technique; doctors and nurses must also consider the human side as well. What’s my bedside manner? How do I share or break bad news? How do I handle an angry patient? Am I speaking in a way that the patient understands?
In the Sim Center, learners interact with standardized patients (SPs). These are actors who portray people with complex personal backstories, medical histories, and symptoms—and who stay in-character throughout the session, reacting to each learner’s questions, approach, and demeanor.
Other hospital functions have benefited from the program as well. “It’s part of our constant effort to improve the care and the safety of our patients,” Augustine said. “SPs can help everyone—even the non-clinical staff—on a care team learn to engage more personally with our patients.”
Want to learn more?
Tune into St. Luke’s Health Now on September 9 at 6:30pm on WFMZ as Augustine and others discuss the fascinating world of SIM!
Have you spotted St. Luke’s Simulation in Motion yet?
The 34-foot Freightliner truck, custom-built for St. Luke’s, means learners no longer must travel to Bethlehem for simulation training. Because the truck comes directly to users, there’s no need to cover shifts, or spend time on the road.
“It’s fully equipped,” Augustine said, “so it provides practically every capability of the actual Sim Center, including SP sessions. It also features A/V recording capabilities; learners can review their procedures in the truck’s debriefing area.”
The truck started traveling around the network in July, and will appear at some community events such as the Diabetes Fun Fair on August 10 at Camp JCC in Center Valley. Visit sluhn.org for more details!



















