Has Skin Cancer Met Its Match?

How one woman beat deadly melanoma, even after it spread to her liver and lungs.
Let’s be honest: Making an appointment with a dermatologist is one of those things we all tend to brush off. Unless there’s an obvious problem—a rash, a super weird new mole that’s popped out of nowhere—the thought of a yearly skin exam probably doesn’t even cross your mind. And that, unfortunately, means that once you or a doctor does notice a problem, things may already be serious.
Take melanoma, for instance. The most deadly form of skin cancer, caused by UV radiation from the sun or tanning beds, kills an estimated 10,130 people in the U.S. every year. If you catch and treat it early, melanoma is almost always curable. If not, the cancer can advance and spread to other parts of the body, where it becomes hard to treat and can be fatal.
If you catch and treat it early, melanoma is almost always curable.
When they hear these statistics, patients are often surprised—and terrified. Lori Riccardi, a 57-year-old kindergarten assistant from York, knows those feelings all too well. Throughout her life, she’d had countless sunburns and never thought to protect herself. So a few years ago, she decided to schedule a dermatologist visit for a head-to-toe skin check and to look into a tender spot on her foot that would often bleed. The doctor removed it and gave her a clean bill of health.
But the spot came back. So she made an appointment with another doctor who biopsied it and scheduled her to see a local surgical oncologist right away. Initially, Lori wasn’t alarmed. She thought it was something that could easily be removed with outpatient surgery. And it was, for the time being. Fast forward a few months, however, and there were other signs of problems including swollen lymph nodes—three of which were cancerous.
Finally, one of Lori’s local doctors recommended an expert that he referred to as the best skin cancer doctor in the region, Sanjiv Agarwala, MD, at St. Luke’s Cancer Center, who frequently conducted clinical trials that might be a good fit for her.
Lori got an appointment and made the two-hour trip to see
Dr. Agarwala the next day. After some tests, they realized they were dealing with Stage 2 Melanoma and that her cancer had spread, which eliminated her from the current clinical trial. So they made a plan to remove some of the cancer, and after a couple months, she was cleared for the next clinical trial.
Of course, as most people would do, Lori sought a second opinion. And when the team at Memorial Sloan Kettering (MSK) in New York told her they concurred with Dr. Agarwala’s care plan, it confirmed what she already knew – he was her guy.
“It’s natural for patients to gravitate toward the biggest name. But many of those big-name places know us now, and I have colleagues there that will refer to us. Patients are surprised when they hear ‘hey, you can go locally for that same treatment.’”
“Our strategy at St. Luke’s is to select clinical trials that really move the needle on cure rates.”
Although he treats other forms of skin cancer, Dr. Agarwala finds melanoma particularly excitingto study because it’s relatively uncommon. “Because it’s rare, you have to collaborate,” he says.
“I work with investigators around the world. It’s a small group of us, so it’s perfectly normal for us to call or text each other. Because we are in constant communication, it allows us to make advances quicker.”
For Lori’s treatment, Dr. Agarwala’s team decided that Keytruda®, a type of immunotherapy specifically indicated for melanoma that has metastasized, would be the logical next step. It was powerful enough to help her own body attack the cancerous cells.
But there were some setbacks and side effects, so soon after, Dr. Agarwala found another type of medication and the right dosing, which is what finally worked for Lori. She’s been on this regimen for a year and a half with no side effects, and all cancer has been kept at bay.
The outcome may have been different for Lori if not for the clinical trial. Nearly all of Dr. Agarwala’s patients are on a clinical trial, and at the end of the day, he says, what matters is finding the right clinical trial for each patient. “It doesn’t matter how many clinical trials you can offer if you aren’t offering the right ones,” he says.
He credits the Clinical Trials team at St. Luke’s for seeking out the best trials and making them available to patients locally. “Our strategy at St. Luke’s is to select clinical trials that really move the needle on cure rates. The advantage of us offering our own clinical trials is that they are built from the ground up and are located right here,” he says. “We can also offer our patients a lot more availability and face-time.”
Now, Lori and her husband of 32 years are back to enjoying their beach house (always sitting under an umbrella with a hat and sunscreen, of course) and spending time with her two adult sons. She gets scanned every three months to monitor for changes, but all is good so far.
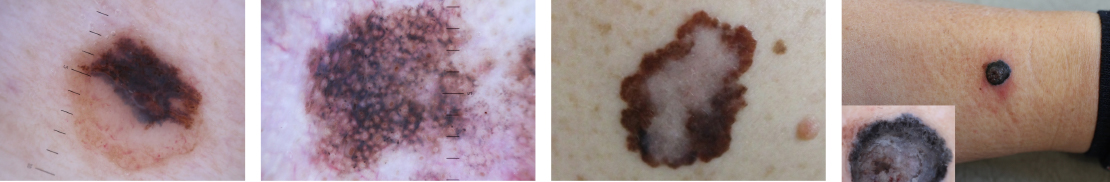
Asymmetry One half does not match the other half.
Border The edges are irregular, ragged, notched or blurred.
Color The color is not the same all over, but may have differing shades of brown or black, sometimes with patches of red, white, or blue.
Diameter The area is larger than a pencil eraser (or is growing larger).
Evolution The evolution of your mole(s) has become the most important factor to consider when it comes to diagnosing a melanoma. Knowing what is normal for YOU could save your life. If a mole has gone through recent changes in color and/or size, bring it to the attention of a dermatologist immediately.
For more information, visit cancer.slhn.org